Evista
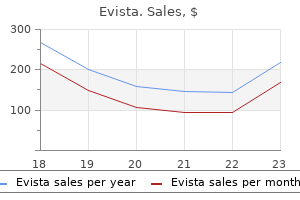
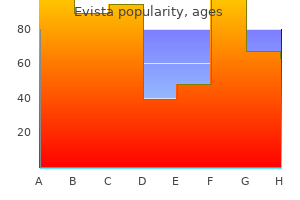
Evista dosages: 60 mg
Evista packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Purchase evista no prescription
Ideally, if wound healing can be completed and maintained, nonoperative administration can be continued for the hindfoot. However, most of these deformities are so severe that salvage surgery turns into necessary in an effort to save the extremity. There are four indications: Non-braceable deformity Chronic ulceration secondary to stress from deformity not responding to bracing Adequate circulation (usually not a problem) Alternative to amputation Preoperative Planning Patients must commit to 5 to eight months of non�weight-bearing and should perceive that problems can happen, corresponding to incomplete therapeutic, an infection, hardware failure, and loss of correction. Amputation have to be accepted as a potential consequence of failure of the process. Emphasis ought to be that the patient will have to have strict management of blood glucose both preoperatively and within the postoperative therapeutic period. Successful revascularization by a vascular surgeon may be necessary to reach the appropriate pressure. The pores and skin is prepared with tincture of iodine and alcohol solution, as Betadine paint prevents Tegaderm from sticking and effectively marking the skin incision. The surgeon should ensure that the anterior superior iliac backbone may be palpated through the drapes. Developing a full-thickness gentle tissue flap and retracting with skin hooks are particularly necessary in this affected person population. In patients with neuropathy, sacrificing the sural nerve as it crosses the sphere helps keep away from extreme dissection and skin retraction. Take care to keep away from damaging the perforating peroneal or anterior tibial arteries during the dissection. If essential, the autograft harvested from the fibula can be mixed with 4-mm cancellous chips. Combine the autograft and allograft mixture with tobramycin (400 mg) and vancomycin (500 mg) powder. The antibiotic bone graft mixture is to be packed between the bony surfaces and to the anterior, posterior, medial, and lateral features of the tibia and calcaneus to facilitate an extra-articular fusion along with the intra-articular fusion. Note the addition of antibiotic powder to the graft (we sometimes use vancomycin and tobramycin). Rigid fixation Complete d�bridement of all synovial and scar tissue Cut the distal tibial floor flat with an oscillating noticed and contour it with a big burr. Denude the calcaneus articular surfaces of cartilage, maintaining as a lot subchondral bone as possible. The posterior aspect may have slight flattening so the tibia will sit secure on the calcaneus with the anterior tibia resting in opposition to the talar neck. Surfaces should be steady but not necessarily flat, as gaps may be filled with bone graft. Preparation of the anterior tibia to include an arthrodesis to residual talar head and neck. The foot must be plantigrade, at ninety degrees with respect to the leg and aligned with respect to the anterior superior iliac backbone, anterior tibia tubercle, and second toe. The hindfoot must be positioned in 5 degrees of valgus, with 5 to 10 degrees of external rotation of the foot. To do that, select the entry level for the blade plate on the junction of the lower and center thirds of the calcaneus, a minimal of 1 cm above the plantar cortex of the calcaneus. Although not often needed, the plate could be contoured to the lateral tibia with the desk plate bender. We have selected the fivehole plate with a 40-mm blade to traverse the width of the calcaneus. Hold the alignment of the tibia on the calcaneus and the anterior tibia on the neck of the talus with the 2. Select an area on the lateral calcaneus on the junction of the center and distal thirds, at least 1 cm above the plantar cortex of the calcaneus and in line with the lateral tibia shaft. Place this in order that the 85-degree-angled plate information portion of the condylar blade information aligns with the tibia and the three-hole drill information sets on the lateral calcaneus preselected entry level for the blade. Hammer the chisel a quantity of centimeters and withdraw until the medial cortex is penetrated. Remove the plate holder and use the impactor to drive and seat the plate into the bone. At this point, bone graft could be added to fill voids between the tibia and calcaneus and the anterior tibia and neck of the talus.
Evista 60 mg
If scapular manipulation is needed to gain better exposure, the rhomboids, trapezius, and dorsal scapular muscular tissues could be divided, allowing the scapula to be mobilized laterally. Visceral injury When approaching from the right aspect, the surgeon ought to dissect the delicate tissues away from the spine as shut as potential to the bone with a blunt gauze or finger to stop injury to the cisterna chyli and thoracic duct. Vascular damage Intercostal neuralgia Atelectasis Neurologic injury Wrong-level surgical procedure Significant bleeding may be encountered when coming into the epidural space. Anterior spinal artery syndrome following belly aortic aneurysmectomy: case report and review of the literature. For retroperitoneal exposures, the approach goes via the stomach wall to the layer of the transversalis fascia and then progresses laterally until this fascia ends, exposing the retroperitoneal fats. For transperitoneal exposures, the transversalis fascia is divided within the midline, as is the peritoneum, and the exposure proceeds immediately posteriorly to the level of the sacral prominence. The abdominal contents are retracted to expose the great vessels overlying the anterior lumbar spine. Vascular the stomach aorta and the bifurcation into the left and proper frequent iliac arteries lies anterior to the venous system, and the left iliac artery is typically encountered first (L4�5). The center sacral artery and vein branch off the left widespread iliac and ought to be ligated or cauterized if small. Exposures above L5�S1, nevertheless, require mobilization of the good vessels to the best. To do that, the iliolumbar vein, which branches off the left widespread iliac, should be identified and ligated (see Techniques section). Genitourinary Left kidney: rarely visualized, surrounded by perinephric fat (L1�2) Left ureter: simply retracted anteriorly with peritoneal contents and could be recognized by stimulated peristalsis Muscular Psoas (paraspinal, L1�L5) Neurologic Sympathetic chain (paraspinal, anterior and medial to psoas) Presacral plexus (directly over sacrum) Lumbosacral plexus (posteromedial to and inside psoas muscle) Genitofemoral nerve (lies on anterior facet of psoas) Lymphatic Paraspinal lymphatics and lymph nodes Lymphatic drainage will seem as a milky white fluid, which is never of clinical consequence. The presence of midline stomach mesh, cellulitis or abscess, and a colostomy are relative contraindications to the anterior method. Previous exposure of the anterior lumbar backbone, significantly if it concerned mobilization of the good veins, makes revision approaches rather more risky as a result of the larger chance of vascular injury. Obesity (body mass index above 40) is a relative contraindication to anterior exposure of the lumbar backbone as a end result of the depth of the operative field. Preoperative ureteral stents can even assist stop ureteral damage during revision exposure. Below (distal to) the arcuate line, the posterior rectus sheath is no longer current. Exposures to the L4�5 disc area usually require identification and incision of the posterior rectus sheath. Anterior corpectomy for tumor resection, radical deformity correction, and vertebral physique osteomyelitis Preoperative Planning When exposure of the L5�S1 disc is required, the direct anterior lumbar strategy must be used in most cases, because the ilium blocks passable entry from a lateral approach. The direct anterior method is less morbid than the lateral method to the lumbar backbone as a outcome of the latter entails greater division of the belly wall musculature. Anterior plates can be used from a direct anterior approach at L5�S1 and in some cases L4�5, depending on the vascular anatomy. However, greater mobilization of the nice vessels at the level of the bifurcation is required from a direct anterior versus lateral strategy. In this case the bifurcation occurs at the stage of the L5 vertebra rather than the L4�5 disc house. This configuration may make entry simpler on the L4�5 disc but more durable on the L5�S1 disc, as the left iliac vein might obliquely cross over it (arrow). Finally, further time and care are required to retract the small intestines; this typically requires extra retractors and enormous sponges to prevent interference during the remainder of the procedure. Right versus left retroperitoneal With sure failures of lumbar disc replacement, revision exposures of the lumbar spine are necessary. To preserve the left retroperitoneal exposure for a potential revision publicity, some surgeons advocate performing a right-sided retroperitoneal incision on the index surgical procedure. Because optimum placement of a lumbar disc correlates with improved functional outcomes for the patient, we advocate performing the exposure that provides the best set of circumstances for accurate gadget placement at the outset. Care should be taken to ensure that the pelvis is stage in order that true anteroposterior and lateral fluoroscopic pictures can be simply obtained.
Buy generic evista
When in doubt, an extensile exposure seems ideal, following the line of neurovascular bundles. Often, the preliminary incision will trigger difficulty with distal path plantar because it included a plantar fascia release. For these events, especially when the majority of symptoms are at the medial plantar nerve entrapment by the abductor fascia, the revision incision must curve anteriorly and at an angle to the original reduce. The pores and skin appears nicely vascularized right here and sharp angles rarely have therapeutic issues. The strategy to the lesser peripheral nerves in the foot and leg normally follows anatomic guidelines. The superficial peroneal nerve may be compressed and adhesive to the peroneal muscle fascia on the supramalleolar stage of the leg. The nerve here often runs in its personal separate sheath and should be instantly visualized to ensure full release. Very little information has been presented concerning barrier procedures for these more purely sensory nerves. The amount of scar tissue formation varies extensively and dictates the tempo of the surgical procedure. Starting extra proximally in "virgin" tissue appears wise as distal dissection proceeds more simply when the nerve and vessels have been identified. The preliminary pores and skin incision ought to be superficial, particularly distally when the nerve moves extra medial and superficial by the lancinate ligament. The posterior tibial nerve could have a venous plexus round it, which could be stripped off with some bleeding. The larger vessels will send small branches by the nerve, and these may have cauterization or ligation depending on measurement. Persistent or vigorous bleeding can often be managed with local pressure distally, but the tourniquet is typically wanted to higher dissect and cauterize the tough venous plexus across the medial plantar nerve. Vessel loops assist with retraction of the vessels and for movement of the nerves with out harm. The dissection must embrace the area above the ankle joint, and dissection proceeds distally past the abductor fascia. The soft tissues ought to yield easily to a small hemostat sliding alongside the nerve, making certain launch. Note the intact vasculature, because the procedure is often carried out without inflation of the tourniquet. A branch can be resected by chopping a small rectangular part of the NeuraWrap around the bigger nerve to allow the branch to exit unimpeded. Most posterior tibial nerve segments require one or two 7 4-mm sections of NeuraWrap. Occasionally the calcaneal branch or the primary branch of the lateral plantar nerve shall be wrapped. Close the subcutaneous tissues rigorously with resorbable suture and close the skin with resorbable suture when attainable to avoid irritation within the postoperative interval. Place a cumbersome cotton wrap across the leg with a medial lateral U-splint and a posterior L-splint of plaster, coated with Coban or elastic wrapping. This material is considerably thicker than the saphenous vein however easier to apply because it can typically be wrapped circumferentially rather than "barber-poled" with the labor-intensive wrap method that the saphenous vein requires. The process can be just like that for the posterior tibial nerve, with careful neurolysis and then wrapping with both autologous saphenous vein or NeuraWrap. The superficial peroneal nerve has been wrapped most frequently, with encouraging results. The chance of vascular injury requires microsurgical devices and loupes (or microscope) out there for repair (or availability of a vascular surgeon if desired). A tourniquet should be on the leg or a sterile one must be close by in case of excess bleeding with the difficult dissection. Incomplete decompression Start extra cephalad in virgin territory if possible to see the nerve more easily as properly as to ensure enough proximal decompression. Distal release must be confirmed by simple passage of an instrument along the medial and lateral plantar nerves.

Cheap evista 60mg visa
Stretching of the retracted muscle is often required via longitudinal traction over about a 10-minute time interval to shut the hole. Place the distal incision, over the region of the rupture and gap, medial to the Achilles tendon. This prevents harm to the sural nerve, which runs 5 mm lateral to the Achilles tendon, and retains the incision away from the posterior side of the heel, where it may rub in opposition to a shoe counter, causing irritation. Proximally, curve the incision centrally and continue it up the posterior midline of the calf as much as the proximal extent of the myotendinous junction. The sural nerve within the calf crosses from lateral to central over the myotendinous junction area and then passes underneath the medial head of the gastrocnemius muscle proximally. The nerve runs with the lesser saphenous vein, which aids in figuring out its location, and the vein too must be preserved if attainable. Carefully mirror the paratenon off the proximal tendon and protect it for later restore. The incision required to handle a uncared for Achilles rupture with a big gap between tendon ends. The sural nerve should be isolated because it traverses from the lateral side of the tendon distally to the posterior midline within the calf. A scar pseudo-tendon is frequently identified inside the rupture hole, and this ought to be resected together with the nonviable ends of the tendon. Leave the underlying muscle fibers intact and hooked up to the proximal muscle physique. Place the apex of the V in the midline at the most proximal portion of the myotendinous junction. The limbs of the V then diverge to exit on the medial and lateral borders of the tendon, respectively. In our experience with these more intensive gaps (greater than 5 cm), we suggest that the limbs of the V are no much less than twice the size of the rupture hole to permit sufficient lengthening to be obtained. Insert the suture into the free end of the tendon and then loop it in a locking sample up the side of the tendon. Attempt to capture about one third to one half of the tendon width with every loop of the suture. Once five loops have been thrown, move the suture via the substance of the tendon, exiting at the same level on the other side of the tendon. Throw another five locking loops towards the tip of the tendon, with the suture exiting once more at the free end of the tendon. This is a firm steady traction, permitting the muscle fibers to gently stretch out and slide. While some pressure is required to create this advancement slide, take patience and great care to not detach the tendon from the muscle, which would devascularize the tendon. While that is being utilized, gently tease the muscle fibers of the myotendinous junction longitudinally, allowing the myotendinous junction to slide distally. Continue traction till the tendon ends could be approximated with the ankle resting pressure matching the unaffected side. The long arm of the inverted Y is the size that the tendon has been elongated-equal to the size of the measured hole. A locking Krackow-type sew is placed in every end of the ruptured tendon, utilizing at least 5 locking loops of braided no. The inverted V is cut through the tendinous portion solely, leaving the underlying muscle fibers intact. The underlying muscle fibers are allowed to slide after the V launch is made in the tendinous portion. A Beath pin is drilled by way of the calcaneus immediately anterior to the Achilles tendon insertion. Traction can be utilized to the suture to hold the tendon throughout the bone tunnel at the applicable pressure. Fix the tendon into the bone tunnel utilizing an interference screw of the same measurement as the bone tunnel.
Diseases
- Gaucher-like disease
- Diabetes mellitus type 2
- Cryptomicrotia brachydactyly syndrome excess fingers
- Chondrodysplasia, Grebe type
- Telencephalic leukoencephalopathy
- Hyperlysinemia
Evista 60mg lowest price
Completeness of the discharge All constructions famous in the description must be fully released. Gentle range-of-motion train of the ankle is re-emphasized to promote gliding of the nerve, but non�weight-bearing continues for two extra weeks. At 4 weeks, the affected person is allowed to bear weight using the customized orthotic described earlier. If the patient fails to comply, pain might be skilled, usually on the dorsum and lateral border of the foot, presumably from "arch strain. Revision Surgery Less predictable results have been reported for revision surgery. Although 73% of patients indicated they had been higher off than before surgical procedure, total satisfaction was reported by solely 27%, and 36% were dissatisfied with the process. In revision conditions, sufferers with evidence of inadequate prior distal tarsal tunnel release and those with persistent mechanical plantar fasciitis are more than likely to have good decision of their symptoms. Data on the usage of collagen conduits and wraps are being collected, with encouraging early outcomes. This is a big enchancment over the less than 50% complete satisfaction reported in most up-to-date research of restricted plantar fascia release with a limited nerve release, or nerve release with out plantar fascia launch. The improved rate of total satisfaction is reflective of the decrease charges of residual ache and exercise limitations. Improved surgical results in primary surgery patients are thought to be due to the great surgical strategy with the objective of addressing all potential sites of pathology-nerve and plantar fascia. Meticulous technique is needed to avoid potential complications, which include wound dehiscence, perineural scarring, and direct nerve injury. Plantar fascia release with proximal and distal tarsal tunnel launch: surgical method to continual, disabling plantar fasciitis with associated nerve pain. Chronic, disabling heel ache with associated nerve ache: primary and revision surgery results. Podium presentation and abstract on the seventeenth Annual Summer Meeting of the American Orthopaedic Foot and Ankle Society, San Diego, July 2001. American Sports Medicine Institute evaluate of 104 feet (92 patients) following the entire plantar fascia and tarsal tunnel release between 1996�2000. Heel pain triad: the combination of plantar fasciitis, posterior tibial tendon dysfunction, and tarsal tunnel syndrome. Effects of tarsal tunnel release and stabilization procedures on tibial nerve tension in a surgical created pes planus foot. The predominant symptom is ache in the plantar area of the foot when initiating strolling. The trigger is a degenerative tear of part of the fascial origin from the calcaneus, adopted by a tendinopathy-type response. Rarely, ache could additionally be situated distally; this situation is recognized as distal plantar fasciitis. Careful comparability to the contralateral heel is useful in confirming tenderness typical for plantar fasciitis. As the toes prolong through the stance section of gait, the plantar fascia is tightened by a windlass mechanism, resulting in elevation of the longitudinal arch, inversion of the hindfoot, and exterior rotation of the leg. Endoscopically, the pertinent anatomy is the abductor hallucis muscle medially, then the plantar fascia. After fasciotomy, the flexor digitorum brevis comes into view as the medial intermuscular septum. Stress fractures, unicameral bone cysts, and large cell tumors are often recognized with plain radiography. Three-phase technetium bone scans are rarely necessary but are constructive in up to 95% of instances of plantar fasciitis. Ultrasound is cost-effective and easily measures the thickness of the plantar fascia, documenting plantar fasciitis when thickness exceeds 3 mm.
Purchase evista 60 mg overnight delivery
Reconstruction of the lateral ligaments of the ankle for persistent lateral instability. The use of arthroscopic thermal shrinkage to treat continual lateral ankle instability in younger athletes. Patients should be asked about ache and its relationship to activity and instability. Pointing to the foot or ankle with one finger will assist focus the patient on the realm of maximum discomfort and focuses the examination. Ankle instability may be difficult for the patient to convey; it might be more subtle than recurrent inversion injuries. Patients ought to be requested if the ankle gives method; if potential, the position of the foot through the instability episode and circumstances (running, chopping left, chopping proper, and so on. The ligament passes superficial to the lateral margin of the posterior side of the subtalar joint and courses deep to the peroneal tendons to insert through a broad base onto the lateral facet of the calcaneus. Osteochondral defects of the talus and peroneal tendon tears are recognized associated pathologies. However, a recurrently unstable ankle treated with acceptable physical therapy protocols may profit from lateral ankle ligament repair or reconstructions. Left untreated, persistent lateral ankle instability might end in fixed varus tilt to the talus throughout the ankle mortise and eventual ankle arthritis. Most sufferers present due to the incapacity associated with the recurrent sprains. Physiotherapy and bracing will enhance signs in some patients with recurrent instability. Recurrent ankle instability may be secondary to tarsal coalition; if the hindfoot is stiff on clinical examination, then calcaneal axial view and normal foot radiographs may establish the coalition. Selective, diagnostic native anesthetic blocks of the ankle, subtalar, or talonavicular joints could additionally be required to determine localized joint ache. When the diagnosis of ankle instability is suspected however stays in query, an inversion stress take a look at done beneath fluoroscopy, in comparison with the physiologically stable contralateral ankle, may be helpful. We take the ankle and hindfoot by way of a spread of movement unbiased of one another to determine the joint of most discomfort. A resisted contraction of ankle eversion must be performed and the tendons palpated for ache and fullness (suggestive of tenosynovitis). The peroneal tendons, which are flexors, are greatest isolated with the ankle in plantarflexion and testing eversion in opposition to resistance. Peroneal tendon weak point accompanies most peroneal pathology because of pain; marked weak spot might signify a peroneal tendon tear. In our experience, the combination of chronic ankle instability, varus hindfoot, and marked peroneal tendon weak spot should elevate the suspicion for a peroneal tendon tear. Occasionally, an equinus contracture could also be associated with lateral ankle instability. A Silfverskiold check (ankle dorsiflexion with the knee flexed contrasted with ankle dorsiflexion with the knee extended) allows the examiner to determine whether or not the contracture is isolated to the gastrocnemius or entails both the gastrocnemius and soleus elements of the Achilles complex. A direct anterior draw (pulling the talus anteriorly with out plantarflexion and inner rotation) might fail to elicit instability in an unstable ankle as an intact deltoid ligament medially will forestall translation. Instead, the examiner should hold the tibia posteriorly with the left hand whereas translating the calcaneus anteriorly and internally rotating the foot on the identical time. Side-to-side comparison to the contralateral, physiologically steady ankle assists in indentifying ankle instability. An damage to the syndesmosis (ie, "excessive ankle sprain") could also be elicited with a squeeze take a look at and by rotating and translating the talus within the ankle mortise in dorsiflexion. A syndesmotic damage must be distinguished from lateral ankle instability since remedy is totally different. We also routinely look at the medial ankle for deltoid instability, since medial and lateral instability may coexist. Patients with recurrent ankle instability may develop peroneal tendon weak spot and loss of proprioception. Bracing might help a affected person to recover from a sprain and prevent future sprains by strengthening the dynamic, stabilizing peroneal tendons. Nonoperative therapy is less effective if ankle instability is related to fixed hindfoot varus.
Discount 60mg evista with amex
In case of tibial malunion, a correction via a supramalleolar osteotomy must be associated with the ankle prosthesis. In case of hindfoot deformity, a correction through a subtalar or triple arthrodesis or calcaneal osteotomy must be carried out in association with the ankle prosthesis. We carry out the triple arthrodesis by what would be an extension of the anterior strategy to the ankle to prepare the talonavicular joint and a restricted lateral�subfibular ap proach to the subtalar joint. We keep away from dissection underneath the talar head to decrease the danger of necrosis of the talar body. Fixation is achieved utilizing a talocalcaneal screw and two talonavicular and calcaneocuboid staples. Graft materials is harvested from an area donor web site (bone slices taken from the midtarsal joint, typically bone material taken from the proximal tibial metaphysis) and in some instances from the ipsilateral iliac crest in case of severe deformity. Bone Loss Implant fixation requires adequate tibial and talar bone stock and an intact ankle mortise. Medial release in a varus deformity is challenging and involves the entire deltoid ligament, which is first released subperiosteally from its malleolar attachment after which indifferent from the talus. We have been glad with this balancing approach, which, in our hands, eliminates the necessity for the medial malleolar osteotomy technique to rebalance the deltoid ligament. A triple arthrodesis was accomplished in association with lateral malleolus correction osteotomy. Forty-five days later, the entire ankle prosthesis was implanted in a appropriately aligned hindfoot. Occasionally, nevertheless, for severe varus malalignment, we have to perform a lateralizing and valgus-producing calcaneal osteotomy to further realign the hindfoot. Ankle Stiffness End-stage tibiotalar joint arthritis nearly at all times results in stiffness of the tibiotalar joint. Stiffness with equinus deformity requires sequential steps to regain dorsiflexion, beginning with excision of anterior ossifications, then liberating of talomalleolar adhesions, and at last posterior capsulectomy from inside the joint. However, nice warning should be used to avoid avulsion of the medial malleolus and accidental penetration of the prepared tibial surface. In explicit, the surgeon must be certain that full capsulectomy is performed on the posteromedial corner, flush with the tibialis posterior tendon. In this case, tenolysis of the tibialis posterior tendon with opening of its retinaculum by way of a restricted posteromedial strategy could also be helpful. This method makes posterior capsular launch and even repair of associated fissures much easier. Lastly, contracture of the triceps surae and Achilles tendon is often answerable for a deficit of dorsiflexion. Therefore, lengthening must be thought of each time dorsiflexion is less than 10 levels after insertion of the trials. Release of flexors could also be achieved through both tendon lengthening or fasciotomy of the triceps surae. Lengthening approach consists of constructing two or three percutaneous staged incisions with a nice scalpel; every incision should contain slightly more than half of the tendon. The most distal incision could also be carried out on both facet, depending on the fibers to be lengthened-laterally for a valgus deformity in order to preserve varus-oriented fibers, and medially for a varus hindfoot. While making incisions, the ankle should be held in pressured dorsiflexion with the trial components in place. The insertional fascia of the gastrocnemius is sectioned in a V-shaped fashion, and the underlying soleus fascia is sectioned according to the muscle fibers. Repositioning of the talar component requires full gentle tissue release (ie, talomalleolar compartment, posterior capsule) as properly as correction of equinus deformity (if any) by way of Achilles tendon lengthening. Should these procedures prove ineffective, the talar component will have to be moved posteriorly, which implies recutting the anterior chamfer. In our expertise, the tibial element should be positioned as far anteriorly as possible beneath the distal tibia. Total ankle substitute: history, evolution of ideas, design and surgical technique.

Purchase cheap evista online
The anterior and anterolateral annulus ought to be palpated by the instrument and by no means violated, or catastrophic vascular damage could happen. Care ought to be taken to not violate the endplates in regions anticipated to load share with the interbody implant as this could make implant placement troublesome and result in settling of the structural graft. Disc house preparation devices (from left to right): left offset, straight, and right offset rasps, ring curette, reverse curette, straight, left, and proper offset curettes. Other instruments not proven might embrace dilators, shavers, osteotomes, and straight and angled pituitary rongeurs. Rotation of the shaver ought to take away endplate cartilage to facilitate arthrodesis. To keep away from violation of the endplates, care have to be taken when working within the interbody region to keep a parallel trajectory to the disc house. Straight (E) and offset (F) curettes maximize the realm of the disc house that might be accessed and facilitate proper endplate preparation. Access to concave disc areas may be facilitated by removing of posterior endplate osteophytes. The surgeon ought to do not neglect that aggressive removing of the posterior lip could result in a higher danger of implant backout with root compression. On completion of the discectomy and endplate preparation, exposed bony endplates ought to be seen on the cephalad and caudal vertebral bodies. To decrease the danger of neurologic injury and postoperative dysesthetic pain, several suggestions ought to be followed through the disc area preparation and graft insertion: Retraction on the neurologic parts must be minimized, and it should be released intermittently throughout the process. Particularly in revision cases, the neurologic elements must be fastidiously mobilized off the floor of the canal and disc house earlier than retraction. Implants must be selected that might be inserted without excessive neural retraction. This could be an issue with use of threaded cylindrical cages because the peak and width of the system should be equal; consequently, a cage of the appropriate top could be too extensive to be safely inserted. The anterior and lateral features of the disc space ought to then be tightly filled with morselized graft material. Several options can be found to be used as morselized graft material, together with autogenous iliac crest bone graft, native bone graft from the removed aspect and lamina, allograft corticocancellous bone, allograft demineralized bone matrix, ceramic bone graft extenders, and bone-inducing substances corresponding to bone morphogenetic protein. The selection of graft ought to rely upon surgeon experience, host elements which will affect fusion, affected person desire, cost, and availability. Graft impactors must be used to maximize the amount of bone that might be positioned into the interbody house. For the method utilizing a central and anteriorly positioned cage, the anterior 25% of the disc area ought to be crammed initially with tightly packed morselized graft materials. Before inserting the precise cage or graft, the trial must be reinserted to verify that the morselized graft has not blocked the pathway for insertion of the structural graft. The implant should then be inserted into the interbody house and positioned anteriorly and as centrally as potential. Vertical cages or grafts placed posteriorly inside the disc space with cancellous graft packed anteriorly. Trial insertion to make certain that the appropriately sized device will match and that cancellous graft packed into the disc house has not obstructed the pathway. Structural graft in place anteriorly with cancellous graft packed in the remaining portion of the disc house. Intraoperative photograph with unilateral posterior morselized graft in place on proper. Postoperative radiograph demonstrating a stable unilateral arthrodesis (white arrow) in the posterolateral area. Assessment of fusion status in the posterolateral region is typically easier than assessing fusion throughout the interbody house. Compression and Posterolateral Grafting With the implant in place, distraction is launched from the spinous processes or pedicle screws. Compression is then applied to the pedicle screw assemble and the locking nuts are finally tightened.
Real Experiences: Customer Reviews on Evista
Ballock, 24 years: Mark the wedge dimension from the measurement obtained above after which rigorously minimize the block in a "pie" or wedge shape, with the cortical facet widest. This allows differentiation between axial deviations: Resulting from asymmetrical wear of the tibial plafond which may be corrected with tibial preparation.
Grimboll, 61 years: Additional cancellous bone graft is positioned over the decorticated laminae and spinous processes and throughout the aspect joint on the fusion levels. For a four-disc�level drawback, two single-level corpectomies may be carried out with an intervening intact vertebra, or a single-level corpectomy with two single-level anterior cervical discectomies and fusions.
8 of 10 - Review by D. Brant
Votes: 65 votes
Total customer reviews: 65
References
- Garcia Garcia A, Somoza Martin M, Gandara Vila P, Gandara Rey JM. A preliminary morphologic classification of the alveolar ridge after distraction osteogenesis. J Oral Maxillofac Surg. 2004 May;62(5):563-6.
- Wang Y, Auger M, Kanber Y, et al: Implementing The Paris System for Reporting Urinary Cytology results in a decrease in the rate of the iatypicali category and an increase in its prediction of subsequent high-grade urothelial carcinoma, Cancer Cytopathol 126:207n214, 2018.
- Nazarian S, Bluemke DA, Lardo AC, et al. Magnetic resonance assessment of the substrate for inducible ventricular tachycardia in nonischemic cardiomyopathy. Circulation 2005;112(18):2821-2825.
- Bedrossian CW, Miller WC, Luna MA. Methotrexate-induced diffuse interstitial pulmonary fibrosis. South Med J 1979; 72(3):313-8.
- Campbell SS, Murphy PJ. The nature of spontaneous sleep across adulthood. J Sleep Res 2007;16(1):24-32.